Articles about the menstrual cycle usually focus on reproduction and period symptoms rather than helping you discover patterns that affect your entire body. While traditional menstrual cycle diagrams depict a stylized cycle and a 28-day timeframe, modern research shows that menstrual cycles vary widely between individuals and in the same person from cycle-to-cycle.²⁻⁴
Using modern tools like wearable technology like the Oura ring can help you identify your menstrual cycle and map how it affects different systems of your body. These insights can help you adapt your routine to each cycle phase. To learn the phases of your menstrual cycle, and how Oura can help you spot the impact, read on.
Look out for an exclusive TouchCare promo code at the end of the article!
"Modern research shows that menstrual cycles vary widely between individuals and in the same person from cycle-to-cycle."
What Are The Phases Of Your Cycle?
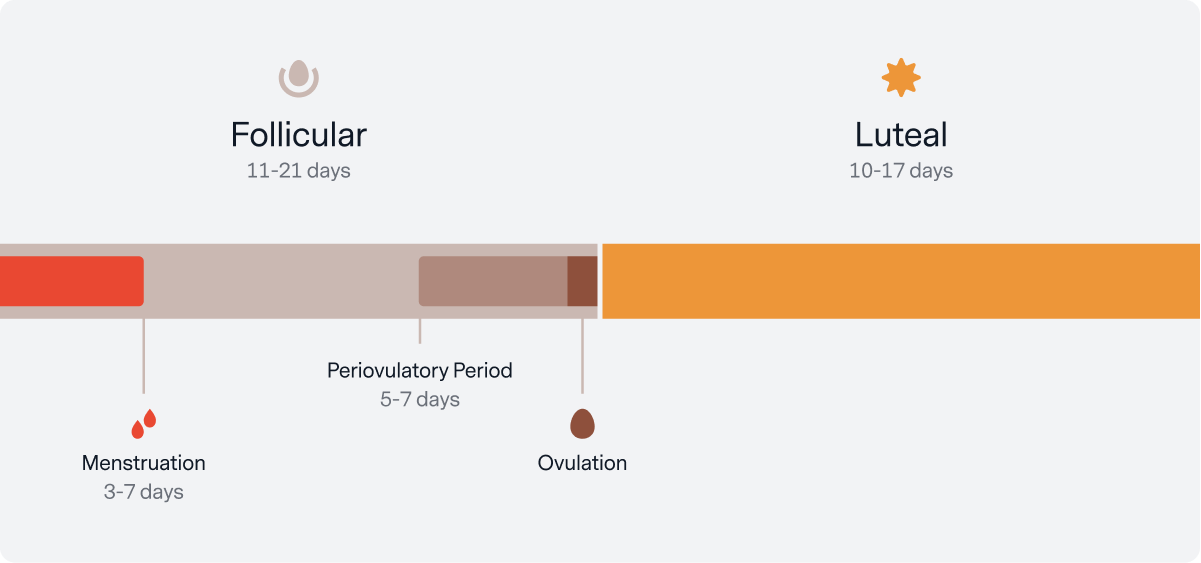
Depending on which articles you read, you’ll see slightly different terms, but they’re all describing the same events: Your follicular & luteal phases.
- Your follicular phase includes menstruation and important events called your “periovulatory period,” which helps your body prepare to release an egg or “ovulate.” Once you ovulate, you shift phases.
- Your luteal phase is your transition to either supporting a pregnancy or starting a new cycle.
The average length, and incredible variability,5-6 of each of these events are shown in the image below.
With each of these events, specific hormones coordinate activity in your reproductive organs, heart⁷,lungs⁸,muscles⁹, brain¹⁰, and other systems in your body. There are many important hormonal players in this process, but we’ll focus on three (estrogen, luteinizing hormone (LH), and progesterone).
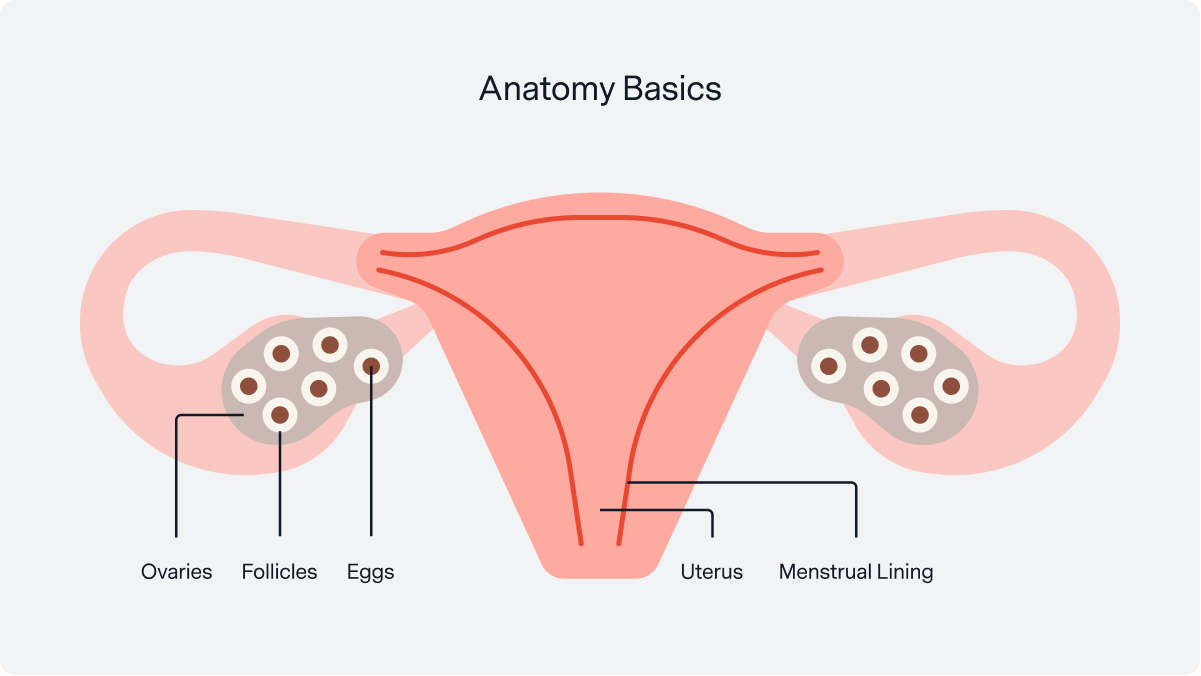
“Follicular” refers to the fact that each of your eggs is contained in a sack within your ovary called a follicle. At the start of this phase, a batch of 20-30 follicles develops on each of your ovaries.¹¹ Around ovulation, one follicle is ‘chosen’ as the dominant egg, while the remaining follicles are naturally broken down. (Don’t worry, you still have ~100,000 eggs even in your mid-20s!)¹²
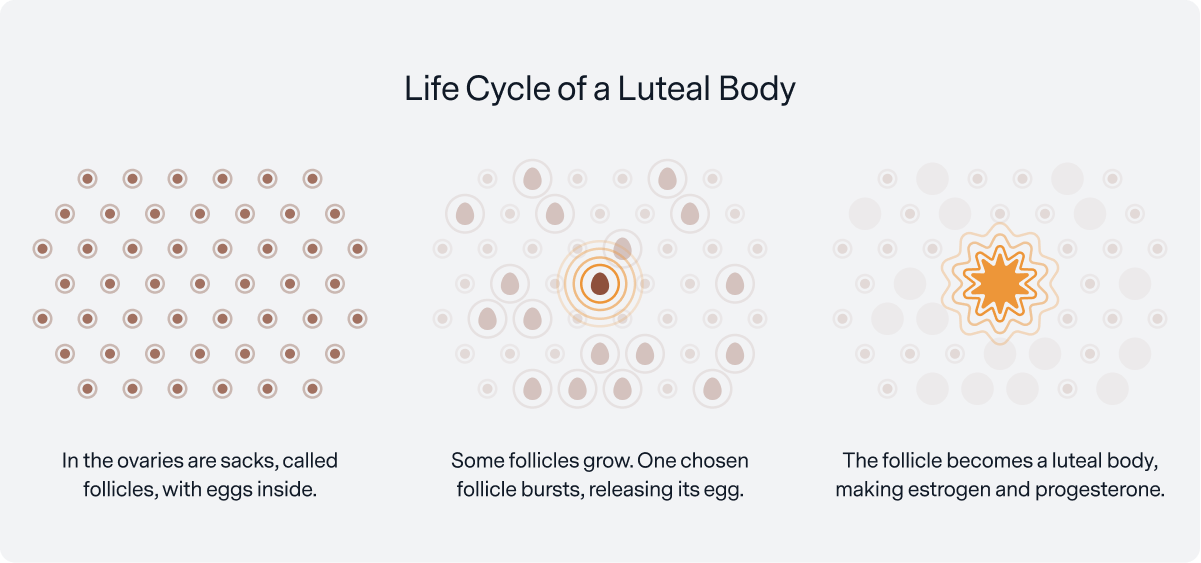
“Luteal” refers to how your chosen follicle becomes a helpful hormone generator after ovulation. Once your follicle releases the egg, the cells in your follicle take on a new purpose; they transform into a luteal body that releases progesterone and estrogen to support a potential pregnancy.
Below, you can see how your hormones relate to your menstrual cycle’s phases. Each hormone peaks in a particular phase: Estrogen during follicular, LH prior to ovulation, and progesterone during luteal.
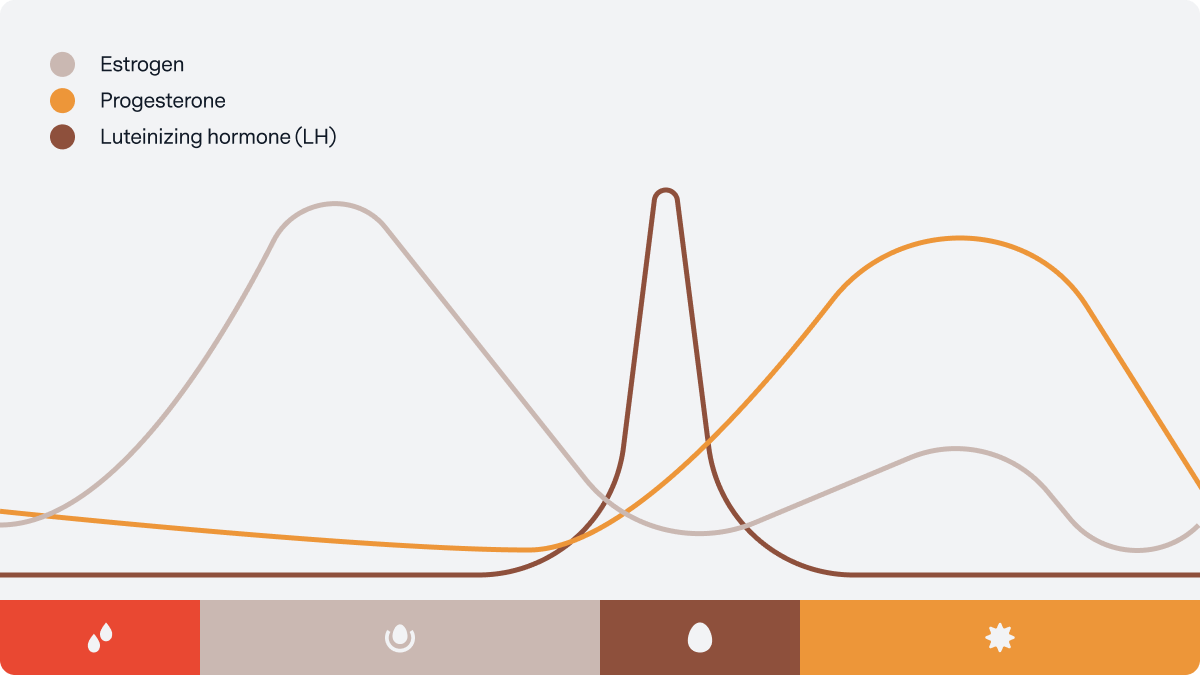
- Menstruation starts your follicular phase with decreasing progesterone, low estrogen, and low LH.
- As your follicular phase continues, your developing follicles produce more and more estrogen.
- Towards the end of your follicular phase, approaching ovulation (your “periovulatory period”), high levels of estrogen, and other factors, set off a flood of luteinizing hormone. This “LH surge” triggers ovulation.¹³
- Your luteal phase starts after ovulation, with your luteal body releasing increasing amounts of progesterone and a small bump in estrogen. As your luteal phase continues, high levels of progesterone thicken the lining of the uterus and prevent contractions.
- Eventually, your luteal body recedes, causing progesterone and estrogen to drop off. As these hormones fall, the top layers of the uterine lining break down and are shed in the form of menstrual bleeding to start a new cycle.
What Patterns Can You Look For?
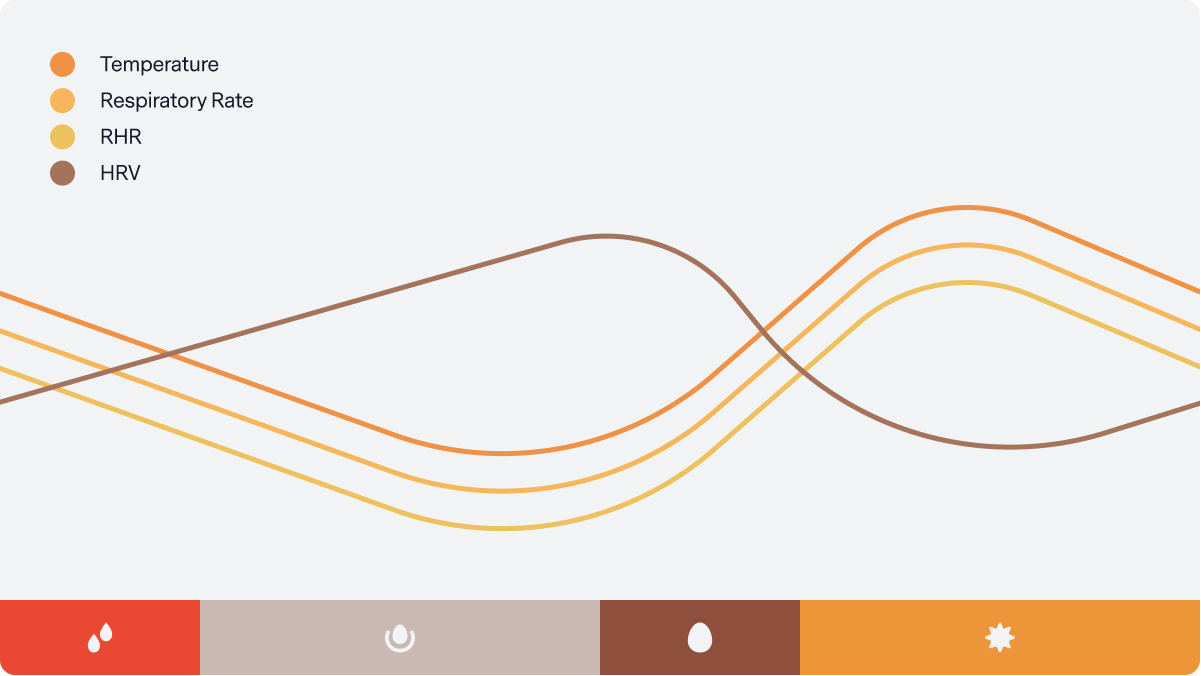
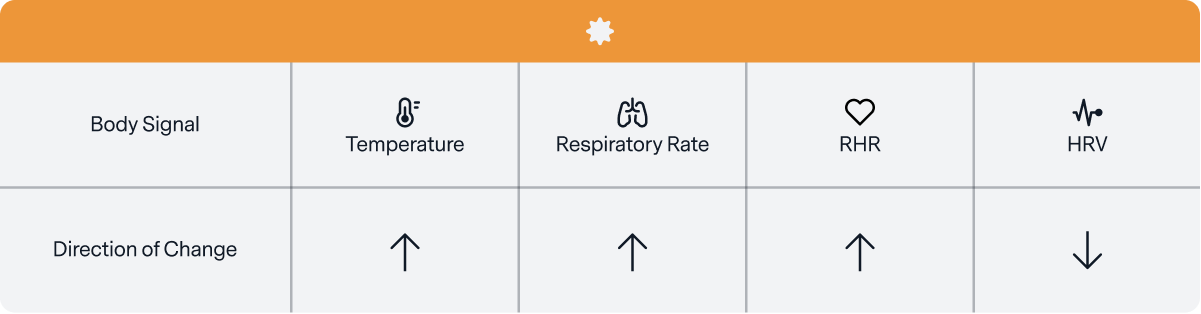
You can spot the timing of these menstrual cycle phases by monitoring the way that hormone fluctuations impact your brain, heart, lungs, reproductive system, and more. These changes show up as patterns in your body temperature, resting heart rate (RHR), heart rate variability (HRV), and respiratory rate.
Keep in mind that these are generalized patterns, and observing your body’s rhythms is your most helpful tool. Avoid comparing your numbers to someone else’s (a ‘high’ temperature or RHR in your luteal phase might be another person’s ‘low’ follicular phase reading). Note that individuals on hormonal birth control will see different trends.
Below is a broad overview of typical patterns:
During Menstruation
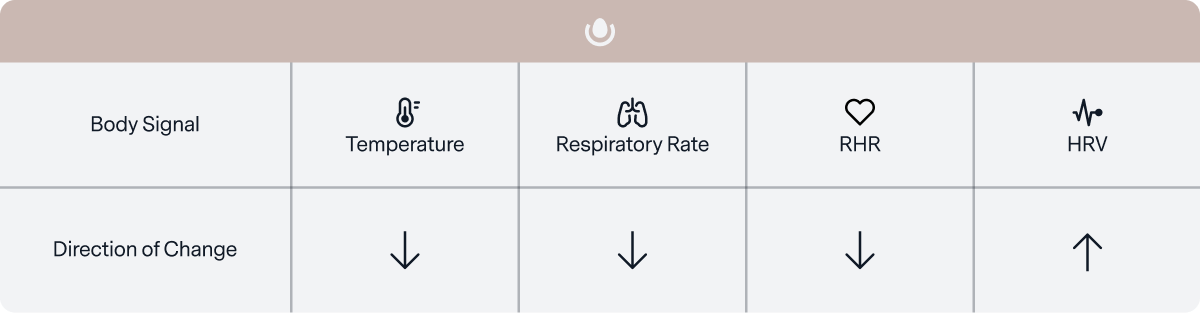
Alongside symptoms like cramping, your menstruation usually signals a return to better sleep¹⁴ and recovery.
At the start of each cycle, progesterone and estrogen decline. This drop in hormones is associated with decreasing RHR and respiratory rate, alongside increasing HRV. The speed at by how quickly your progesterone and estrogen decrease in a given cycle.
Your body temperature is also highly impacted by estrogen and progesterone. Although there are some complex dynamics at play, generally, estrogen decreases your temperature while progesterone raises it. With falling progesterone levels during menstruation, you’re likely to see your temperature decrease.

During The Majority of Your Follicular Phase
Your follicular phase may support peak athletic performance¹⁵⁻¹⁶ and sociability.¹⁷⁻¹⁹ Although there is still more research to be done, higher estrogen levels during the follicular phase may also boost cognition and creativity.²⁰⁻²²
As a group of your follicles develop, they produce increasing amounts of estrogen, and your uterine lining rebuilds to create the best environment for a potentially fertilized egg. This increase in estrogen also affects your heart, lungs, and muscles, resulting in a lower temperature, RHR, and respiratory rate, alongside higher HRV. Although the research is still emerging, these trends, which you might already associate with feeling “better,” may also promote improved athletic performance.²³
Around Ovulation
As your body builds up momentum to release an egg, you may experience a disruption that leaves you feeling out of sorts for a day or so.²⁴
High estrogen levels and other factors set off a cascade across your brain and body that results in an LH surge, which triggers ovulation. The phrases “LH surge” and “ovulation” are often used interchangeably—but these events are actually distinct, with the LH surge almost always happening first! Look out for this common misconception when reading about cycles.
So, what does this mean for fertility? The LH surge and ovulation make up part of your “fertile window,” the time during the menstrual cycle when you may become pregnant (typically 5-7 days).
Around ovulation, these changes can cause rising temperatures, RHR, and respiratory rate alongside declining HRV.²⁵ This is also the time when many women experience “mittelschmerz,” an achy abdominal sensation that scientists think indicates contractions in the fallopian tube as it begins transporting your egg towards your uterus.
During Your Luteal Phase
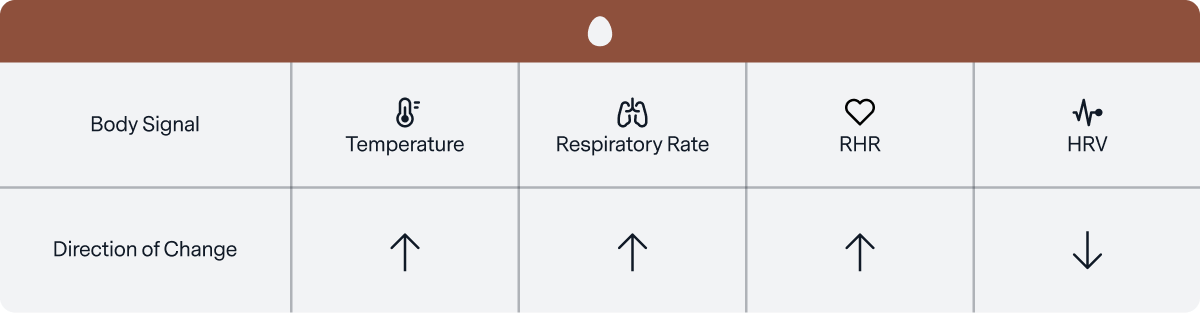
During your luteal phase, you are likely to experience hotter temperatures,²⁶ a higher metabolism, lower energy,²⁷ and a desire to prioritize comfort and rest.₂₈
Early in this phase, your now-empty follicle transforms into a luteal body, which produces increased levels of progesterone and delivers a bump in estrogen. Your LH levels decrease, and the lining of your uterus starts to thicken as a landing pad for a potentially fertilized egg.
Across this phase, rising progesterone increases your body temperature and the activity in your fight-or-flight system. This activity interacts with systems across your body and can be spotted in an elevating RHR, temperature, and respiratory rate, alongside declining HRV.
As your luteal phase continues, your body reaches a turning point:
- If your egg is fertilized, your body prepares for pregnancy and progesterone rises even higher, causing the extra high temperatures you can spot in early pregnancy.²⁹⁻³⁰
- If your egg is not fertilized, progesterone and estrogen drop off again and your cycle restarts. As you get closer to your next menstrual period, the trends listed above will level off as these hormones decline.
For many, the decline in estrogen and progesterone as the luteal phase transitions into menstruation can manifest negatively. Individual experiences vary widely by symptom and intensity.³¹ This is the time when people may experience breast tenderness, fluid retention, bloating, cramps, cravings, mood swings, tiredness, or anxiety, collectively known as “PMS” (premenstrual syndrome).
Why Cycles Vary & Why It’s Important to Understand Yours

Cycle phases change from person to person and cycle to cycle, and one individual might ovulate earlier or have an extended luteal phase compared to another. You might ovulate on day 15 one cycle, and day 18 the next. It’s even normal to have a cycle that skips ovulation, an “anovulatory cycle,” from time to time.³²
These wide ranges highlight how important it is to understand your personal cycle because, if you’re aiming to avoid pregnancy or land your fertility target, a shift in a single phase can make a big difference.
Keep in mind that your cycle length may also change over time.³³ Past birth control usage is associated with cycle irregularities during recovery and younger women tend to have longer cycles.³⁴⁻³⁶ Moreover, factors like your genetic background, body composition, and exercise habits may also influence your cycles.³⁸⁻⁴⁰ And, even with all these current insights, there are many more patterns yet to be discovered.
Using Oura to Understand Your Cycle
Because the Oura Ring measures your RHR, HRV, respiration, sleep, and body temperature, it can be a helpful tool for spotting your cycle and discovering its impact on your body. If you’re interested in gaining personalized health insights about your sleep, activity, health (and more!), click here for an exclusive promo code!
References
- https://www.netterimages.com/menstrual-cycle-unlabeled-rehabilitation-75638.html
- Direito A, Bailly S, Mariani A & Ecochard R (2013). Relationships between the luteinizing hormone surge and other characteristics of the menstrual cycle in normally ovulating women. Fertil Steril 99, 279–285.e3.
- Bull, J. R., Rowland, S. P., Scherwitzl, E. B., Scherwitzl, R., Danielsson, K. G., & Harper, J. (2019). Real-world menstrual cycle characteristics of more than 600,000 menstrual cycles. NPJ digital medicine, 2(1), 1-8.
- Mihm, M., Gangooly, S., & Muttukrishna, S. (2011). The normal menstrual cycle in women. Animal reproduction science, 124(3-4), 229-236.
- Fehring, R. J., Schneider, M., & Raviele, K. (2006). Variability in the phases of the menstrual cycle. Journal of Obstetric, Gynecologic & Neonatal Nursing, 35(3), 376-384.
- Najmabadi, S., Schliep, K. C., Simonsen, S. E., Porucznik, C. A., Egger, M. J., & Stanford, J. B. (2020). Menstrual bleeding, cycle length, and follicular and luteal phase lengths in women without known subfertility: A pooled analysis of three cohorts. Paediatric and Perinatal Epidemiology, 34(3), 318-327.
- Brar, T. K., Singh, K. D., & Kumar, A. (2015). Effect of different phases of menstrual cycle on heart rate variability (HRV). Journal of clinical and diagnostic research: JCDR, 9(10), CC01.
- Driver, H. S., Mclean, H., Kumar, D. V., Farr, N., Day, A. G., & Fitzpatrick, M. F. (2005). The influence of the menstrual cycle on upper airway resistance and breathing during sleep. Sleep, 28(4), 449-456.
- Oosthuyse, T., & Bosch, A. N. (2010). The effect of the menstrual cycle on exercise metabolism. Sports medicine, 40(3), 207-227.
- Toffoletto, S., Lanzenberger, R., Gingnell, M., Sundström-Poromaa, I., & Comasco, E. (2014). Emotional and cognitive functional imaging of estrogen and progesterone effects in the female human brain: a systematic review. Psychoneuroendocrinology, 50, 28-52.
- Silber, S. J. “Beating Your Biological Clock”.
- Silber, S. J. “Beating Your Biological Clock”.
- Direito A, Bailly S, Mariani A & Ecochard R (2013). Relationships between the luteinizing hormone surge and other characteristics of the menstrual cycle in normally ovulating women. Fertil Steril 99, 279–285.e3.
- Romans, S. E., Kreindler, D., Einstein, G., Laredo, S., Petrovic, M. J., & Stanley, J. (2015). Sleep quality and the menstrual cycle. Sleep medicine, 16(4), 489-495.
- Pallavi, L. C., SoUza, U. J. D., & Shivaprakash, G. (2017). Assessment of musculoskeletal strength and levels of fatigue during different phases of menstrual cycle in young adults. Journal of Clinical and Diagnostic Research: JCDR, 11(2), CC11.
- Julian, R., Hecksteden, A., Fullagar, H. H., & Meyer, T. (2017). The effects of menstrual cycle phase on physical performance in female soccer players. PloS one, 12(3), e0173951.
- Krug, R., Finn, M., Pietrowsky, R., Fehm, H. L., & Born, J. (1996). Jealousy, general creativity, and coping with social frustration during the menstrual cycle. Archives of sexual behavior, 25(2), 181-199.
- Sundström Poromaa, I., & Gingnell, M. (2014). Menstrual cycle influence on cognitive function and emotion processing—from a reproductive perspective. Frontiers in neuroscience, 8, 380.
- Montero-López, E., Santos-Ruiz, A., García-Ríos, M. C., Rodríguez-Blázquez, M., Rogers, H. L., & Peralta-Ramírez, M. I. (2018). The relationship between the menstrual cycle and cortisol secretion: Daily and stress-invoked cortisol patterns. International Journal of Psychophysiology, 131, 67-72.
- Toffoletto, S., Lanzenberger, R., Gingnell, M., Sundström-Poromaa, I., & Comasco, E. (2014). Emotional and cognitive functional imaging of estrogen and progesterone effects in the female human brain: a systematic review. Psychoneuroendocrinology, 50, 28-52.
- Hara, Y., Waters, E. M., McEwen, B. S., & Morrison, J. H. (2015). Estrogen effects on cognitive and synaptic health over the lifecourse. Physiological reviews, 95(3), 785-807.
- Krug, R., Stamm, U., Pietrowsky, R., Fehm, H. L., & Born, J. (1994). Effects of menstrual cycle on creativity. Psychoneuroendocrinology, 19(1), 21-31.
- Julian, R., Hecksteden, A., Fullagar, H. H., & Meyer, T. (2017). The effects of menstrual cycle phase on physical performance in female soccer players. PloS one, 12(3), e0173951.
- Brott, N. R., & Le, J. K. (2019). Mittelschmerz. In StatPearls [Internet]. StatPearls Publishing.
- Buxton, C. L., & Atkinson, W. B. (1948). Hormonal factors involved in the regulation of basal body temperature during the menstrual cycle and pregnancy. The Journal of Clinical Endocrinology, 8(7), 544-549.
- Buxton, C. L., & Atkinson, W. B. (1948). Hormonal factors involved in the regulation of basal body temperature during the menstrual cycle and pregnancy. The Journal of Clinical Endocrinology, 8(7), 544-549.
- Tada, Y., Yoshizaki, T., Tomata, Y., Yokoyama, Y., Sunami, A., Hida, A., & Kawano, Y. (2017). The impact of menstrual cycle phases on cardiac autonomic nervous system activity: an observational study considering lifestyle (diet, physical activity, and sleep) among female college students. Journal of nutritional science and vitaminology, 63(4), 249-255.
- Romans, S. E., Kreindler, D., Einstein, G., Laredo, S., Petrovic, M. J., & Stanley, J. (2015). Sleep quality and the menstrual cycle. Sleep medicine, 16(4), 489-495.
- Buxton, C. L., & Atkinson, W. B. (1948). Hormonal factors involved in the regulation of basal body temperature during the menstrual cycle and pregnancy. The Journal of Clinical Endocrinology, 8(7), 544-549.
- Smarr, B. L., Zucker, I., & Kriegsfeld, L. J. (2016). Detection of successful and unsuccessful pregnancies in mice within hours of pairing through frequency analysis of high temporal resolution core body temperature data. PloS one, 11(7), e0160127.
- Matsumoto, Tamaki, Takahisa Ushiroyama, Mina Morimura, Toshio Moritani, Tatsuya Hayashi, Takashi Suzuki, and Noriyuki Tatsumi. “Autonomic nervous system activity in the late luteal phase of eumenorrheic women with premenstrual symptomatology.” Journal of Psychosomatic Obstetrics & Gynecology 27, no. 3 (2006): 131-139.
- Direito A, Bailly S, Mariani A & Ecochard R (2013). Relationships between the luteinizing hormone surge and other characteristics of the menstrual cycle in normally ovulating women. Fertil Steril 99, 279–285.e3.
- Bull, J. R., Rowland, S. P., Scherwitzl, E. B., Scherwitzl, R., Danielsson, K. G., & Harper, J. (2019). Real-world menstrual cycle characteristics of more than 600,000 menstrual cycles. NPJ digital medicine, 2(1), 1-8.
- Gnoth, C., Frank-Herrmann, P., Schmoll, A., Godehardt, E., & Freundl, G. (2002). Cycle characteristics after discontinuation of oral contraceptives. Gynecological Endocrinology, 16(4), 307-317.
- Bracken, M. B., Hellenbrand, K. G., & Holford, T. R. (1990). Conception delay after oral contraceptive use: the effect of estrogen dose. Fertility and sterility, 53(1), 21-27.
- Nassaralla, C. L., Stanford, J. B., Daly, K. D., Schneider, M., Schliep, K. C., & Fehring, R. J. (2011). Characteristics of the menstrual cycle after discontinuation of oral contraceptives. Journal of Women’s Health, 20(2), 169-177.
- Bull, J. R., Rowland, S. P., Scherwitzl, E. B., Scherwitzl, R., Danielsson, K. G., & Harper, J. (2019). Real-world menstrual cycle characteristics of more than 600,000 menstrual cycles. NPJ digital medicine, 2(1), 1-8.
- Harlow, S. D., Campbell, B., Lin, X., & Raz, J. (1997). Ethnic differences in the length of the menstrual cycle during the postmenarcheal period. American journal of epidemiology, 146(7), 572-580.
- Leeners, B., Geary, N., Tobler, P. N., & Asarian, L. (2017). Ovarian hormones and obesity. Human reproduction update, 23(3), 300-321.
- Pauli, S. A., & Berga, S. L. (2010). Athletic amenorrhea: energy deficit or psychogenic challenge?. Annals of the New York Academy of Sciences, 1205, 33.
- Baker, F. C., & Lee, K. A. (2018). Menstrual cycle effects on sleep. Sleep medicine clinics, 13(3), 283-294.
- Pengo, M. F., Won, C. H., & Bourjeily, G. (2018). Sleep in women across the life span. Chest, 154(1), 196-206.
- The Endocrine Society. “In healthy young women, sleep quality varies throughout the menstrual cycle.” ScienceDaily. www.sciencedaily.com/releases/2019/03/190323145156.htm (accessed December 20, 2019).
Inhale. We've got this. Exhale.
Understanding healthcare; with us, it’s personal.
